Here’s a fun little question for you – which one of these statements is true?
A) A Banyan Tree near Kolkata, India is larger than the average Walmart
B) There are more nerve connections in your brain than there are stars in our galaxy
C) Heartburn is usually due to too little stomach acid, not too much
Okay, that was a trick question. They’re all true. (1) Now, maybe you’re thinking, “That can’t be right. I’ve taken an antacid when I had heartburn and it helped, so clearly the issue was too much acid.”
That’s certainly what I thought when I was one of the 60 million Americans struggling with heartburn. However, according to Jonathan Wright, M.D., author of Why Stomach Acid Is Good For You, the “Chances are very high – over 90 percent – that the real culprit is actually underproduction of stomach acid.”
Unfortunately, the most popular form of over-the-counter medications – proton pump inhibitors – “are not the benign drugs the public thinks they are,” says Dr. Shoshana J. Herzig of Harvard Medical School. (2)
We’ll dive into why later in this article, plus what Dr. Wright says is the true cause of most heartburn, but first I want to mention that none of these statements have been evaluated by the FDA, this article is not medical advice, and it is not meant to diagnose or treat any condition. I’m just a former heartburn sufferer passing along information I’ve found helpful from respected physicians, clinical studies conducted by places like Johns Hopkins University, and articles from Scientific American and the Mayo Clinic.
Please talk with your healthcare provider about what approach to heartburn is best for you. Now that we’ve got that out of the way, let’s dive in.
So if antacids aren’t reducing excess acid, what are they actually doing?
According to Dr. Wright, who has worked with thousands of heartburn patients at the Tahoma Clinic:
“stomachs are built for the very purpose of containing and working with very strong acid, acid that is one-hundred-thousand times stronger than the acidity of our blood.” (3)
Our stomach acid plays an essential role in helping us break down food so that nutrients can be absorbed, and also kills a variety of bacteria, parasites, and other pathogens on contact. When levels are normal, individuals are very unlikely to experience heartburn symptoms such as a bitter, acid taste in the mouth or a burning sensation in the throat or behind the breastbone.
However, if acid levels are low, the chances increase. Here’s why:
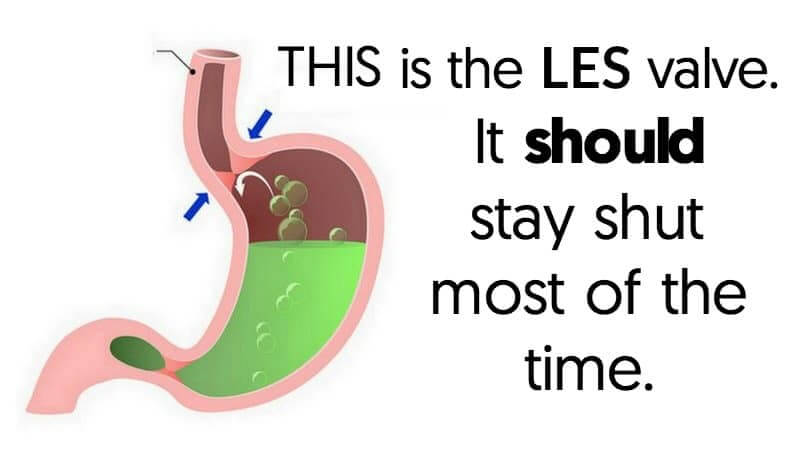
Just above the stomach there is a valve called the lower esophageal sphincter (LES) – it protects the esophagus from harsh stomach acid. When the LES is functioning normally, it only opens when you eat, drink, belch, or (yep) vomit.
If the LES is working properly, it doesn’t matter how much acid we have on our stomachs. It’s not going to make it up to the esophagus. On the other hand, if the LES is asleep at the switch, even a small amount of acid could reflux into the esophagus under the right conditions. Scientists have found that when we have heartburn or GERD, the LES opens briefly when it’s not supposed to. If we’ve got acid – or anything else – in our stomachs, sometimes even a little bit, and it happens to be in the vicinity of the LES when it pops open inappropriately, we get reflux.” (3)
So what causes the LES to malfunction?
After testing the gastric pH of thousands of heartburn sufferers at his Tahoma Clinic, Dr. Wright has concluded that in 90%+ of cases it’s low stomach acid that is causing LES malfunction.
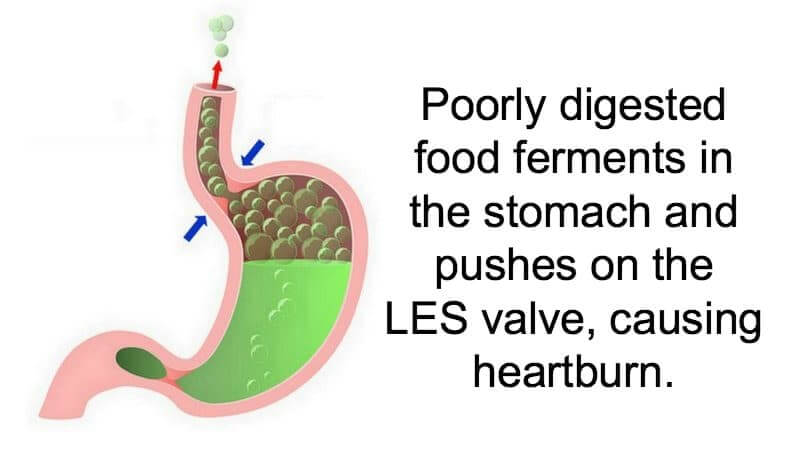
Remember, in addition to breaking down food so that nutrients can be absorbed, stomach acid also provides an “acid barrier” that kills bacteria, parasites, and other pathogens in our food.
If the acid is too weak, poorly digested food – especially carbohydrates – can become a source of nourishment for these bacteria/pathogens. As they feed, they produce fermentation byproducts (gases) that create pressure in the stomach and push on the LES valve. When the pressure builds, some acid may be pushed through the LES into the esophagus, causing heartburn.
Stomach acid levels tend to drop as we age, so if heartburn were caused by too much of it you’d think this would mostly be an issue for kids and teens. Of course, it’s the opposite.
That’s not to say teens can’t have low stomach acid – I actually got my first prescription for heartburn when I was nineteen. But on the whole, we tend to have more problems with heartburn as we get older despite dropping levels of stomach acid.
Dr. Wright’s “argument is with the mistaken concept that it takes ‘too much’ stomach acid to do the damage. Even a small amount of acid in the wrong place (such as the esophagus) can cause symptoms and ultimately tissue damage. (After all, we know that stomach acid is strong stuff, if it can help reduce a tough beefsteak into the equivalent of beef soup in an hour or so.)” (3)
In some cases a hiatal hernia – which is when the upper part of the stomach bulges through the large muscle separating the abdomen and chest – can also cause LES dysfunction. For some people chiropractic care may be able to ease the stomach back into its proper place, and in other cases surgery may be required.
Hiatal hernias can be diagnosed with an endoscopy, which allows the doctor to look at the area directly or an X-ray that requires the patient to take barium (which is a heavy metal). Personally, I’d opt for the endoscopy.
Calcium channel blockers can also lower esophageal sphincter tone, making the LES more susceptible to dysfunction. (4)
Common Causes of Low Stomach Acid
- Age (levels tend to drop over time)
- Stress, particularly the chronic type, can inhibit the body’s secretion of hydrochloric acid (stomach acid). (5)(6)
- Certain gut infections, such as H. pylori and candida, reduce the body’s production of hydrochloric acid (7) It can be argued, however, that these infections only take hold if gastric acid secretion is already compromised. From that perspective, the presence of these microbes simply further inhibits the production of hydrochloric acid.
- A mutation in one of the genes that influences gastric acid production (8)
- Use of antacid medications
Heartburn Medication Concerns
Most of us tend to think of heartburn medications as pills that just “take the edge off” and leave us with normal acid levels. Unfortunately, not only can they reduce levels that may already be too low, sometimes they almost completely eliminate it.
The drug most commonly prescribed for heartburn today, Prilosec, virtually eliminates acid in the stomach around the clock, a fact that is proudly promoted in the drug’s widespread consumer-oriented advertising. Prevacid, Aciphex, Protonix and Nexium do about the same thing.” (3)
Although eliminating stomach acid will relieve symptoms of indigestion, it also prevents the stomach from doing its job – digesting food and killing pathogens as they enter our system. When taken long-term – which is defined as more than one year by the FDA – heartburn medications may cause side effects such as decreased resistance to infection, nutritional deficiencies and an increased risk of certain diseases.
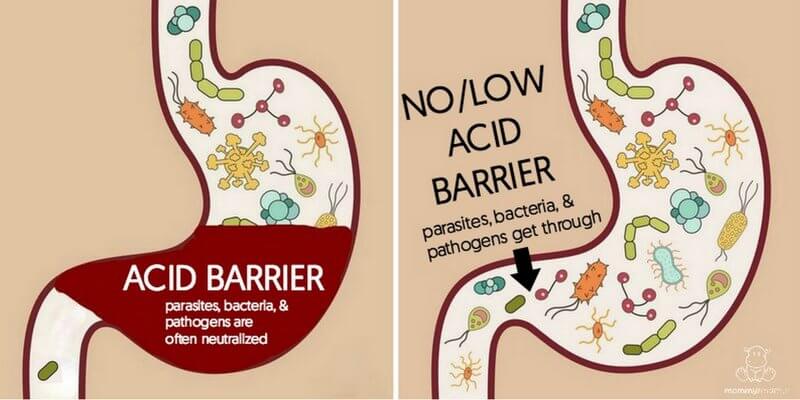
Impaired Resistance To Infection
As we covered earlier, the stomach is supposed to be an “acid barrier” that protects against intestinal tract infection. Unfortunately, according to John Clarke, a gastroenterologist at Johns Hopkins Hospital in Baltimore, lowering stomach acid using proton-pump inhibitors like Nexium, Prilosec and Prevacid “leaves people vulnerable to nutritional deficiencies and infections, including food poisoning like salmonella, a serious, sometimes life-threatening digestive system infection called Clostridium difficile, and perhaps pneumonia.” (9)
Other studies have found individuals who take acid suppressing drugs have an increased risk of getting pneumonia. (10)
Dr. Wright tells this story:
Here’s an extreme, but very revealing, incident: Decades ago, public health officials in India investigated why some people in a village in the midst of a cholera epidemic didn’t contract the disease, while others did. They found that more of those who stayed healthy had normal levels of stomach acid, while those that developed the disease usually did not. Apparently, the strong stomach acid killed the bacteria before it could ‘colonize’ (and damage) the entire gastrointestinal tract.” (3)
Decreased Nutrient Absorption
Stomach acid helps to cleave vitamins and minerals away from dietary fats, proteins, and carbohydrates. Without it, our bodies don’t break nutrients down in absorbable pieces, which can lead to deficiencies – even when someone is eating a very healthy diet. Studies have found connections between acid blocking medications and low levels of:
- Vitamin B-12 (11)
- Vitamin C (12)
- Iron (12)
- Magnesium (2)
Conditions Associated With Low Stomach Acid
Inadequate levels of stomach acid have been associated with a number of health conditions, including:
- Allergies (13)
- Anemia (13)
- Asthma (13)
- Autoimmune diseases such as Rheumatoid arthritis and Graves disease (13)
- Chronic kidney disease (14)
- Dementia (15) (16)
- Heart attack (17)
- Heartburn/acid reflux
- Skin issues such as acne, eczema or psoriasis (13)
- Small intestine bacterial overgrowth (SIBO) (18)
- Stomach cancer (19)
Research suggests low stomach acid may also increase the risk of:
- Diabetes (20)
- Chronic liver disease (21)
- Osteoporosis (22)
Lifestyle Changes That May Help
According to Dr. Jonathan Wright, “In cases of mild to moderate heartburn, ‘acid indigestion,’ bloating, and gas, actual testing for stomach acid production at Tahoma Clinic shows that hypochlorhydria (too little acid production) occurs in over 90 percent of the thousands tested since 1976.
In these cases, a ‘natural strategy’ is almost always successful.” (3)
You’ll find the details of his approach in this article.
This article was medically reviewed by Madiha Saeed, MD, a board certified family physician. As always, this is not personal medical advice and we recommend that you talk with your doctor.
Want more research-backed natural remedies?
No problem, I’ve created a free ebook for you – Kitchen Apothecary: 25+ Natural Remedies Using Ingredients From Your Pantry – as a gift for signing up for my newsletter. You’ll also get updates when I post about safe essential oils for pregnant/breastfeeding mamas, exclusive gifts and coupons (I was able to give away a jar of free coconut oil to anyone who wanted it recently!), plus other goodies.
Sign up using the form below.
Sources
1. Insider (2014) 17 Crazy Facts That Sound Fake But Are Actually True
2. New York Times (2015) Taking Heartburn Drugs Long-Term
3. Wright, Jonathan (2001) Why Stomach Acid Is Good For You
4. Seretis, Charalampos et. al. (2012) Calcium Channel Blockers and Esophageal Sclerosis: Should We Expect Exacerbation of Interstitial Lung Disease?
5. Esplugues, J. V. et. al. (1996) Inhibition of gastric acid secretion by stress: A protective reflex mediated by cerebral nitric oxide
6. Kelly G. Lambert and Craig H. Kinsley (2010) Clinical Neuroscience: Psychopathology and the Brain Second (2nd) Edition
7. Brzozowski, Tomasz et. al. (2005) Influence of gastric colonization with Candida albicans on ulcer healing in rats: effect of ranitidine, aspirin and probiotic therapy
8. Science Daily (2008) Gene That Helps Control Production Of Stomach Acid Discovered
9. NPR (2016) Popular Heartburn Pills Can Be Hard To Stop, And May Be Risky
10. Laheij, Robert J. F. et. al. (2004) Risk of Community-Acquired Pneumonia and Use of Gastric Acid–Suppressive Drugs
11. Mayo Clinic. Heartburn medicines and B-12 deficiency
12. Heidelbaugh, Joel J. (2013) Proton pump inhibitors and risk of vitamin and mineral deficiency: evidence and clinical implications
13. Medical News Today. What is hypochlorhydria?
14. Washington Post (2016) Popular heartburn medication linked to chronic kidney disease
15. New York Times (2016) Heartburn Drugs Linked To Dementia Risk
16. Science Daily (2020) Newly discovered mechanism can explain increased risk of dementia
17. Stanford Medicine (2015) Some heartburn drugs may boost risk of heart attack, study finds
18. Dukowicz, Andrew C. et. al. (2007) Small Intestinal Bacterial Overgrowth
19. New York Times (2017) Heartburn Drugs Linked To Stomach Cancer Risk
20. Diabetes Research & Wellness Foundation. Stomach acid could protect people from type 2 diabetes
21. National Institutes of Health (2017) Blocking stomach acid may promote chronic liver disease
22. Pentti Sipponen and Matti Härkönen (2010) Hypochlorhydric stomach: a risk condition for calcium malabsorption and osteoporosis?