Inside: Although seemingly unrelated, symptoms like hives, nausea, a racing heart, sleep issues and digestive problems can be an indication of histamine intolerance. In this post we’ll cover what histamine intolerance is, plus key strategies that may help.
Have you heard the old saying, “If it walks like a duck and quacks like a duck it might NOT BE A DUCK?”
Yeah, me neither. And yet that’s probably the best way to describe histamine intolerance. The symptoms are similar to an allergic reaction, but allergy tests come back negative.
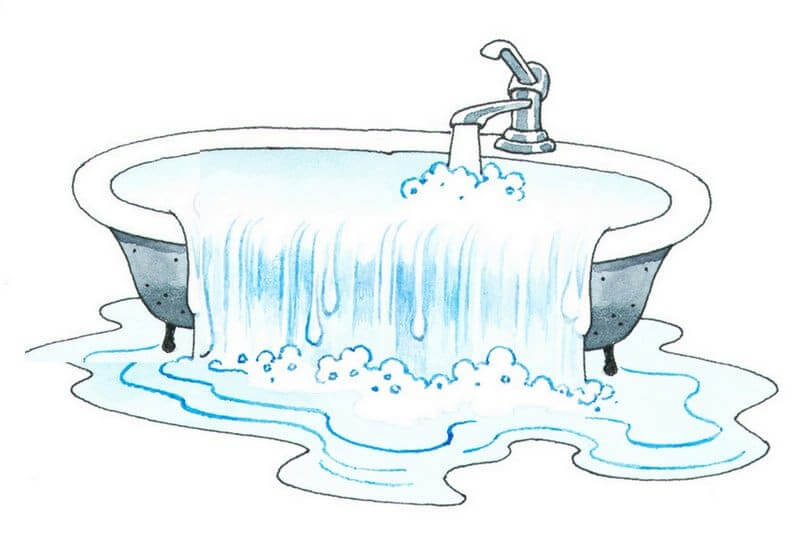
We’re talking headaches, flushing, or hives after eating a meal . . . and maybe also stomach aches, nausea, a racing heart and/or anxiety. Also, it’s common to try removing foods to see if your symptoms improve, only to find that the foods you replace them with seem to cause similar issues.
I dove deep into researching histamine intolerance a few years ago when a family member was struggling with it. There was a lot of trial and error involved, and I know how overwhelming it can feel to try to understand everything. That’s why I’ve collaborated with Nutritional Therapy Practitioner Jordan Hoefing to help you understand the basics, including which foods to avoid and supplements that may be helpful.
Also, in case you’re wondering, after implementing the strategies below, my family member no longer experiences what she calls “histamine overwhelm” – yay!
As always, please keep in mind that this article is for informational purposes only and is based on the opinions of the authors. It is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Please see my full disclaimer here. Okay, let’s get started!
What is histamine and what does it do?
We’ve all seen antihistamine commercials – you know, the ones that always seem to feature a woman dancing in a field of flowers – but few of us know what histamines actually are.
Basically, they’re compounds that the body makes in response to a perceived attack on the immune system. This most often occurs if you eat something you’re allergic to or if you suffer from seasonal allergies. Histamines live in our mast cells (white blood cells), which are responsible for fighting off invaders. Mast cells are somewhat like an ant hill: when you step on an ant hill, (invader) the ants (histamines) rush out of the top of the mound (mast cell) to protect their home underground (your body).
Histamines also act as neurotransmitters, which are chemical messengers that allow our brain and our bodies to communicate and regulate important functions. Histamines belong to the same class, “small molecule neurotransmitter substances”, of neurotransmitters as Serotonin, Epinephrine (adrenaline) and Dopamine.
This aspect of histamines plays a key role in many different functions. Some examples are stomach acid production, setting off an inflammatory (allergy) response, circadian rhythm regulation and creating muscle contractions. In addition, histamines can also impact our mood and state of mind. We will talk more about common symptoms of high histamine levels later in this post.
What is histamine intolerance?
Histamines normally don’t cause issues, but sometimes people produce too many or have a difficult time breaking them down. Think of your body as a bathtub, histamines as water and your ability to break them down as the drain.
If the drain is clogged or the water is coming in too fast for the drain to keep up, the tub will eventually overflow. The point at which histamine intolerance occurs is when the bathtub overflows and you start experiencing symptoms. Unfortunately, you can have dramatically reduced function and it will still take a long time before your “bathtub” overflows. This delayed response makes histamine intolerance difficult to diagnose early on.
By now you’re likely asking, ‘What’s clogging my drain?’ Histamine is mainly broken down in the body by two enzymes: diamine oxidase (DAO) and histamine N-methyltransferase (HMT). DAO is found in epithelial cells in our digestive tract and therefore breaks down histamines that are introduced by the foods we consume. HMT works solely in our central nervous system. Studies have found that DAO metabolizes the bulk of histamines that our bodies have to clear. It is believed that most people who are histamine intolerant have insufficient DAO. (Manzotti et. al.)
Common symptoms of histamine intolerance
- Hives, itching, flushing
- Anxiety
- Headaches
- Runny nose
- Blocked nose (rhinitis)
- Congestion
- Digestive distress (diarrhea, gas, intestinal cramps, heartburn)
- Nausea
- Sensation of heart racing
- Fatigue
- Disrupted sleep
- (Maintz et. al., Joneja)
What causes high histamine levels?
So far, we’ve considered what histamine is and how it affects the body, now let’s focus on what causes elevated histamine levels:
Genetic Mutations – Some individuals have impaired production of the DAO or HNMT enzymes due to genetics.
Histamine-Rich Foods – you’ll find detailed information about these below. The amount of histamines we consume greatly impacts the levels in our body.
DAO Inhibitors – Next on the list are foods that lower DAO (the enzyme that breaks down histamine) function in the body – alcohol, black tea, and green tea for example. Kombucha, which is fermented tea, is another beverage that increases histamine levels by impeding DAO’s effectiveness. Another factor you can control is the use of certain medications. Dr. Joneja states that medications directly affecting inflammation (aspirin, NSAIDS, and antibiotics), will also affect histamine levels. (Joneja)
Gut Dysfunction / Leaky Gut – Remember, one of the primary enzymes that breaks down histamine – DAO – is made in the gut wall. When the wall is damaged and leaky, the body’s ability to produce DAO is diminished. Genetic factors can also interfere with the production or function of the enzymes that metabolize histamine.
So, can I just take antihistamines?
It seems like it would solve everything, doesn’t it? Unfortunately, there are four types of histamine receptors in the body:
- H1 – When histamine binds with these receptors, it creates symptoms such as hives, broncho-constriction, motion sickness, flushing and seasonal allergies. It also makes you more alert, which is why antihistamines that block this receptor are associated with drowsiness.
- H2 – Histamine interaction with these receptors causes the release of gastric acid. When histamine levels are excessive it can cause diarrhea and other forms of digestive upset.
- H3 – When histamine binds with these receptors it affects the central nervous system by downregulating the production of certain neurotransmitters. (Esbenshade et. al.)
- H4 – Interacts with histamine to regulate immune response, including the direction of mast cells and inflammation (Zampeli et. al. )
Antihistamines don’t prevent the production of histamine – they just block histamine from binding with the H1 (and sometimes H2) receptors that cause us to experience certain symptoms. The body still produces histamine, and it can still have negative effects as it attaches to the H3 and H4 receptor sites. (IUPHAR/BPS)
In addition, when we take antihistamines often, our body may sense that the message it’s trying to send isn’t getting through and therefore dial up the production of histamine even more. This can cause a “rebound effect,” where the symptoms of histamine come back strong as soon as the antihistamines wear off. (Lam)
One other thing to consider is that some antihistamines inhibit our body’s ability to make the DAO enzyme, which helps break down histamine. (SOP)
Is it possible to support histamine breakdown?
Absolutely! The important thing to remember is that histamine intolerance is best addressed with complementary methods of healing.
Think of your body as a fine tuned machine with multiple small systems all working together to create one larger system. They all must be running smoothly for the machine to work properly. Focusing on one aspect of healing will get you far, but it’s best to work from multiple angles. Let’s take a look at some key strategies.
1. Follow A Low-Histamine Diet
Let’s go back to our bathtub analogy. When symptoms are present it’s often a sign that the bathtub is overflowing. Following a low-histamine diet is like turning the faucet down. It’s still important to figure out what’s clogging the drain and remove it, but following a low histamine diet reduces the load the body has to clear.
Some foods are naturally high in histamine and certain food preparation techniques – fermentation, for example – increase histamine. There’s a detailed section below on following a low histamine diet, so keep reading!
2. Heal And Seal Your Gut
Poor gut health limits how much DAO enzyme can be made in the digestive tract, so healing and sealing the gut is an important step toward optimizing DAO enzyme production.
This could include eradicating SIBO, candida, a parasite, and identifying possible food sensitivities. I don’t have a lot of confidence in most food sensitivity panels, but I do think the ones offered by Cyrex Labs are helpful. For more information on food sensitivity testing, check out this podcast transcript from Chris Kresser, LAc.
Important note: Bone broth is considered essential in most gut healing protocols, but unfortunately long-simmered broths are high in histamine. Many people, however, have found that broth made in a pressure cooker is well tolerated. Here’s my Instant Pot bone broth recipe.
3. Be Kind To Your Adrenals
Your body’s ability to deal with stress is especially important when dealing with histamine intolerance. Stress activates our immune system, which triggers histamine release. On the flipside, elevated histamine levels trigger a stress response, so it can become a cycle of chronic stress and histamine escalation.
When we experience chronic stress, it puts a burden on our stress-response system (the HPA axis, which is often referred to as the adrenals) and causes the body to focus on survival instead of healing.
Adding self care to the top of your list can go along way in healing your adrenals and body. Here are 15 ways to be kind to your adrenals.
In addition, spending quality time with family and friends, changing your perspective on daily stressors, and simply filling your own buckets with the things you enjoy are also excellent ways to take care of yourself.
4. Supplements That May Help
- Histamine Block From Seeking Health – This supplement contains the DAO enzyme that breaks down histamine in the gut. Umbrellux DAO is another option.
- ProBiota HistaminX From Seeking Health – Unlike most probiotics that can make histamine issues worse, this probiotic contains specific strains that help to break down histamine.
- HistaminX – Contains a blend of herbs and extracts that help to balance the body’s inflammatory and immune responses.
What is a low histamine diet?
It is difficult to formulate a “safe” list of foods for histamine intolerant folks. It’s common to find discrepancies in lists of high histamine containing foods because there are many factors affecting the histamine level of a particular food – how fresh it is, for example.
The most common problematic foods are fermented foods, long-simmered foods like 3 day bone broth, gluten (for its ability to permeate the gut), and leftovers that have been sitting for a day or two. Below you’ll find a list of foods to give you an idea of where to start, but you’ll need to listen to your body and make adjustments as needed.
Foods To Avoid
- Fermented foods: alcohol, yogurt, milk kefir, sauerkraut, water kefir
- Aged cheese
- Dried fruits
- Certain fruits like citrus and strawberries
- Certain vegetables = avocados, tomatoes, spinach, eggplant
- Smoked and cured meats including bacon, salami, & sardines
- Vinegar
- Deli meats (preservatives)
- Artificial colors
- Packaged meals ie: frozen meals
- DAO blockers: black and green teas, kombucha
But instead of focusing on what you can’t have, let’s put a spin on it. Here are some amazing foods to embrace:
Foods To Enjoy
- Fresh meats
- Fish that has either frozen in the U.S. or EU, or has been gutted and cooked within 30 minutes of the time it was caught,
- Fresh fruits (except those listed above)
- Fresh vegetables (except those listed above)
- Grains like white rice and oats if tolerated
- Fresh herbs
- Plain nuts and seeds
- Coconut
- Coconut oil, butter, lard, tallow
- Plain coffee is okay according to Dr. Joneja (source)
In addition to low histamine foods, it’s also important to pay attention to histamine liberators. Histamine liberators release histamine inside the gut.
Be mindful with leftovers as well. As food sits, it produces histamines so leftovers aren’t best to rely on when considering a low histamine diet. It’s best to immediately freeze any leftovers into individual portions.
Regarding overcooked foods like bone broth: As mentioned above, bone broth is considered essential in most gut healing protocols, but unfortunately long-simmered broths are high in histamines. Many people, however, have found that broth made in a pressure cooker is well tolerated. Here’s my Instant Pot bone broth recipe. If available it would be beneficial to add pastured chicken feet or other cartilage containing parts to the stock in order to ramp up the gut healing properties of broth.
This article was medically reviewed by Madiha Saeed, MD, a board certified family physician. As always, this is not personal medical advice and we recommend that you talk with your doctor.
Want to dive deeper?
Whew, we made it! If you found this article helpful but want to dive deeper into understanding histamine intolerance, I highly recommend reading this book by Dr. Joneja.